The Changing Relationship Between PBMs and Pharmacies
Compliance, efficiency, and operational effectiveness can be viewed as three of the pillars that help LTC pharmacies hold themselves aloft in a complex and unpredictable market. The first of these is particularly important and extends not only to government regulations but also the stipulations of essential third-party business partners. Pharmacy benefit managers (PBMs) hold perhaps the most sway in this regard.
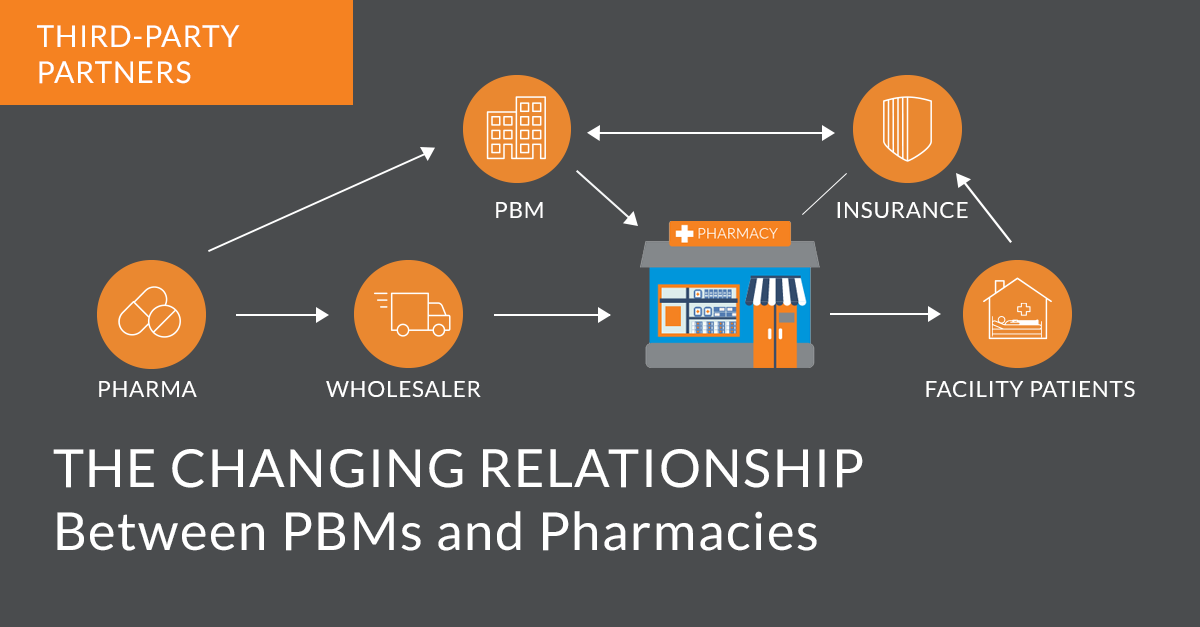
Administrators and technicians alike play pivotal roles in the interactions between LTC pharmacies and their PBMs. This not only entails meeting the demands required by the latter but also means working to understand their broader role in the drug supply chain. Doing so will be critical for the establishment of strong working relationships between PBMs and LTCs.
The PBM position in the pharmaceutical ecosystem
An LTC pharmacy functions as a broker, helping facilities provide their patients with essential medications made by both brand-name and generic drug suppliers. PBMs serve a similar function, standing between insurance payers, pharmacies, and pharmaceutical companies to negotiate medication prices that, in theory, all parties involved will consider fair.
Organizations in the PBM realm play the role described above for companies providing private insurance, employer-subsidized health benefits, and federal Medicare Part D programs, as noted by The Commonwealth Fund. Because insurance payers are footing the bill for PBM services in an attempt to protect their bottom lines, PBMs do a great deal to make sure that medication services are as financially advantageous to insurers as possible. This includes everything from the creation of formulary lists to the implementation of tiered copay structures. PBMs also receive rebates from drug manufacturers which they, in turn, pass along to insurers and patients in the form of discounts. Drug manufacturer rebates help to make expensive brand-name medications more affordable. from.
Every PBM, of course, is protecting its own bottom line, just as pharmacies look to safeguard theirs. It's an understandable impulse. But this can sometimes spin out of control for LTC pharmacies if any of the PBMs they deal with become overzealous in their efforts.
Audits and other risks
In a guest post for law news blog JD Supra, attorney Nick Oberhiden of the firm Oberheiden P.C. explained that PBMs will initiate an audit of any pharmacy that is billing insurance companies in a way the PBM finds odd (or, in serious cases, downright suspicious). The point of the audit is to uncover any errors or omissions on the claim record. If this investigation finds evidence of over-billing, the pharmacy will be held liable through financial retractions. These contractually mandated revocations of claim payments can rise as high as five, six, or even seven figures in some cases. If serious misconduct is found, the pharmacy under audit may have its contract with that insurer terminated immediately.
Everything described above, in a vacuum, isn't particularly strange, nor is it necessarily improper. Pharmacy-PBM contracts typically include audit provisions specifying which records can be examined during audits and requiring auditors to provide proper advance notice.
But according to the National Community Pharmacists Association, PBMs — which, in some states, aren't subject to any kind of licensure requirements or other regulations — have earned some criticism for their usage of power. In certain cases, auditors have cited errors that were typographical or administrative as violations of PBM standards that merited retraction of payment. While in no way an illegal or noncompliant act, some pharmacies may feel as if such penalties were imposed without any examination of context. Pharmacy administrators can challenge PBM audits in civil suits, but such proceedings aren't guaranteed to succeed and will be costly and lengthy no matter what.
PBMs under scrutiny
Despite PBMs' mostly unchecked authority on matters like audits, they have drawn more attention than ever before in the past several years. A majority of American states have passed laws banning gag clauses — rules that prevented pharmacies from telling patients about situations where it would be cheaper to pay for drugs without insurance — and Congress instituted a federal ban in late 2018, per another Commonwealth Fund report.
Then, in July 2020, former President Donald Trump issued an executive order aimed at minimizing what PBMs could earn in drug rebates from manufacturers for any medications provided through Part D plans. (The Department of Health and Human Services finalized the order as an effective regulation in November, and the agency under the administration of President Joe Biden has expressed no intent to rescind it as of February 2021.)
Finally, in December 2020, the Supreme Court ruled unanimously in favor of the state of Arkansas over the Pharmaceutical Care Management Association, a lobbying group representing American PBMs. According to Healthcare Dive, Arkansas legislatures had passed a law forbidding PBMs from reimbursing pharmacies below the wholesale cost paid to acquire drugs from manufacturers. The SCOTUS endorsement of the state's law could potentially lead to the passage of similar legislation elsewhere in the U.S. or even prompt Congress to draft a federal statute.
The path to cooperation between PBMs and pharmacies
While it's probably for the best that PBMs are subject to more regulation now than they were less than half a decade ago, the organizations nonetheless serve a key role in the pharmaceutical supply chain. There is no reason for pharmacy-PBM relationships to be wary or adversarial.
PBMs and pharmacies should have transparent and cordial conversations from the early stages of negotiations onward. This increases the chances of agreement on a direct contract that is favorable to both parties. PBMs would, for example, do well to promise transparency in their operations in return for pharmacies adopting practices and tools that best ensure the most accurate and efficient billing possible. A data-driven and versatile pharmacy management solution like FrameworkLTC will be ideal for pharmacies looking to remain compliant with PBM billing guidelines.